Updated by Piper Wenzel, BS April 2024
Background
- Also known as glomus vagale paraganglioma, vagal body tumor, vagal chemodectoma, glomus vagale
- Rare benign tumor arising from "paraganglionic tissue within the vagal nerve's perineurium" (Ozdemir 2024)
- Most common tumor of post-styloid parapharyngeal space (Ikram 2024)
- Can cause vocal cord paralysis leading to hoarseness and mass effect (Ikram 2024)
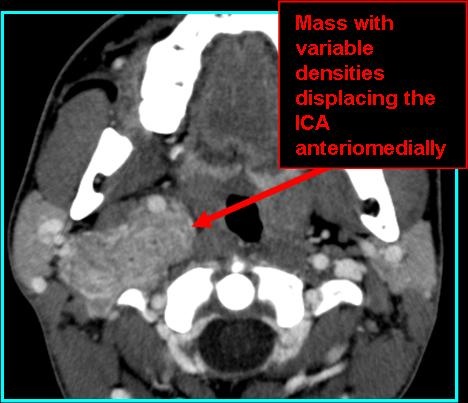
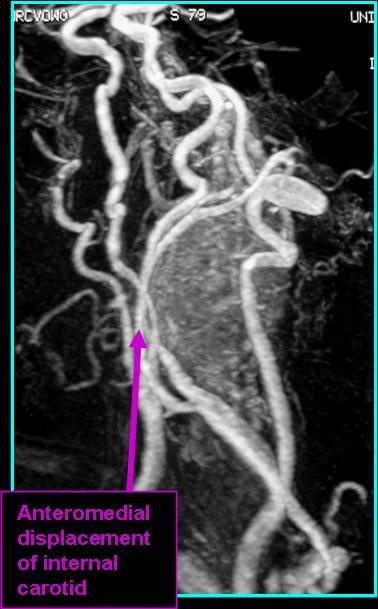
- Pushes internal jugular vein posterolaterally, pushes internal carotid artery anteromedially (Ikram 2024)
- Treatment is generally surgical excision; may result in speech and swallowing deficits (Ozdemir 2024)
Radiologic Findings
- CT and MRI are sensitive due to increased vascularity (Ikram 2024)
- On CT: muscle density with non-contrast; intense enhancement with contrast
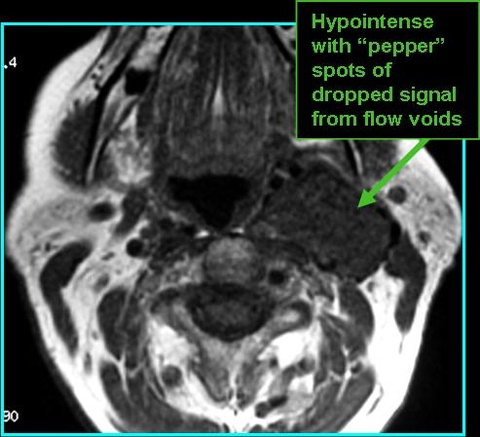
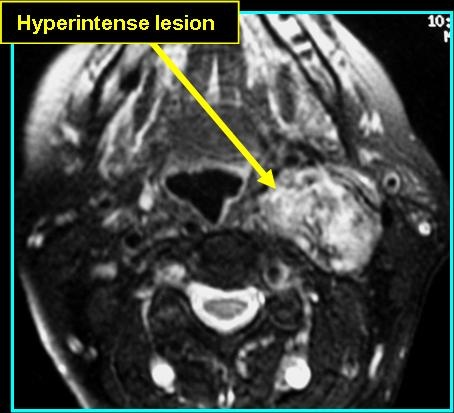
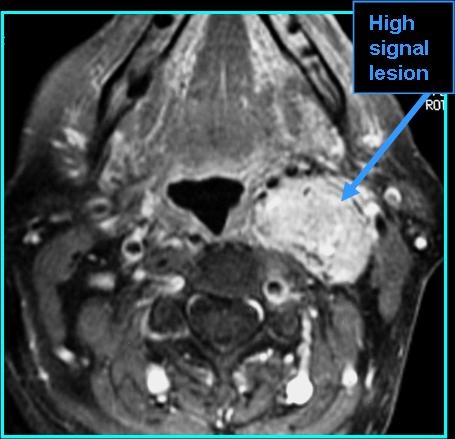
- Look for enhancement on CT with contrast and "salt and pepper" appearance on T1 MR
- On MR: "pepper" (black dots) and "salt" appearance (white dots - uncommon) on T1, hyperintense and good spread definition on post-contrast T1
References
Ozdemir NG, Yilmaz H, Atci IB, Karaoglu AC, Turk O, Gedik AA, Kocak A. Parapharyngeal Prestyloid Vagal Paraganglioma. Turk Neurosurg. 2024;34(1):167-170. doi: 10.5137/1019-5149.JTN.40702-22.2. PMID: 37846532.
Ikram A, Rehman A. Paraganglioma. 2022 Sep 5. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 31751024.