Indications
- Esophageal dysphagia
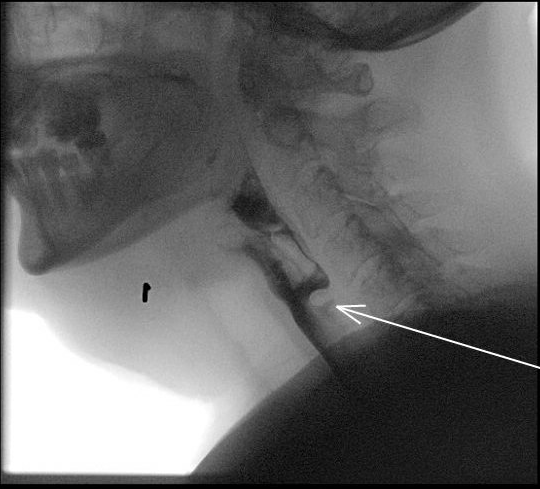
- Cricopharyngeal bar (hypertrophy of the cricopharyngeus muscle)
Procedure
- Orotracheal intubation (tube off to the right in the gutter)
- Paralysis OK (succinylcholine)
- Maxillary mouth guard
- Turn 90 degrees from anesthesia, generally no shoulder roll
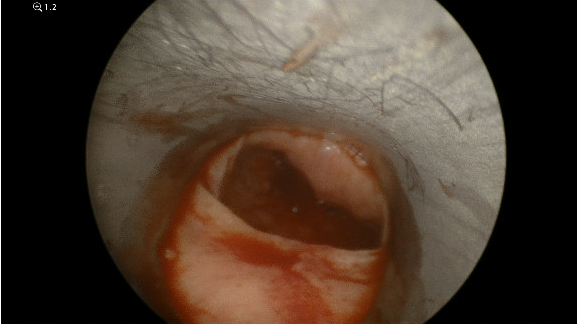
- Perform rigid esophagoscopy first with photodocumentation
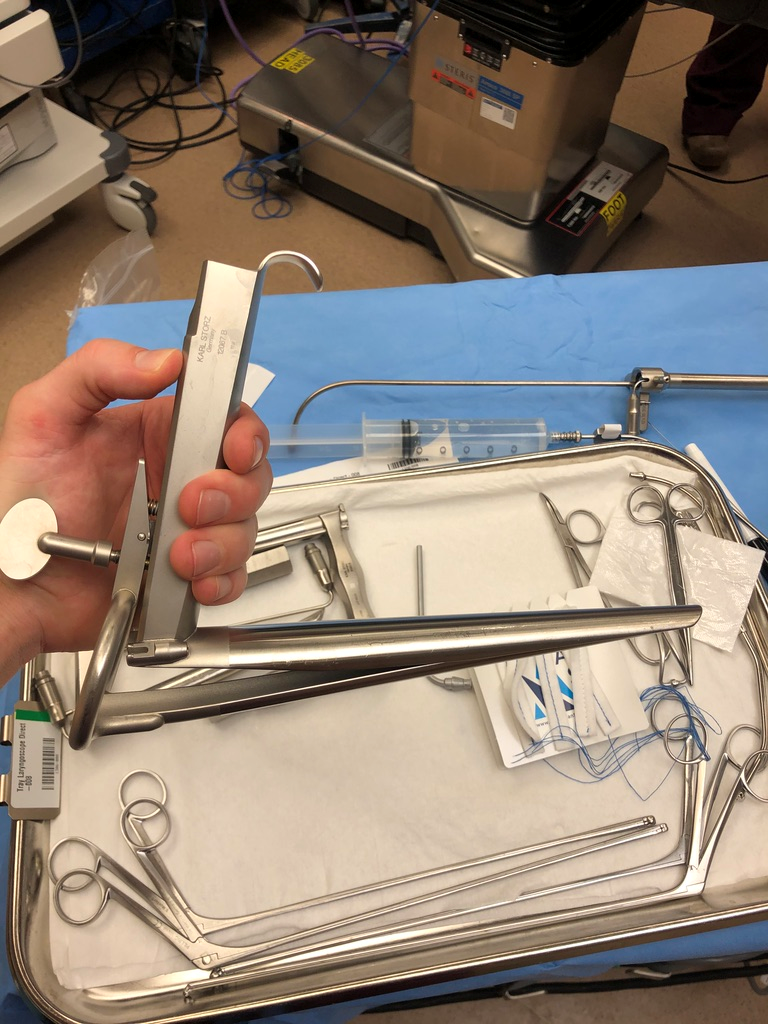
- Weerda Diverticuloscope or Benjamin Hollinger Diverticuloscope to expose cricopharyngeal bar
- Place in suspension
- Can use Kleinsasser laryngoscope as a backup if can't get exposure with diverticuloscope (may be too short)
- 100 units of botox - add 1 cc of normal saline to dilute to 100 U/cc
- Trease injector - microlaryngeal injection instrument
- Inject ~ 0.3 cc in the left, middle and right of the cricopharyngeal bar (total of 33 U per area)
- Maloney esophageal dilators - start around 48 Fr and advance to 56 Fr
- Tip - much easier to advance Maloney dilators into the esophagus with the laryngoscope in place to anteriorly displace the tongue
Sample Operative Note
The patient was escorted to the OR by the anesthesia team. A pre-induction checklist was performed. General anesthesia was induced, and the patient was orotracheally intubated by the anesthesia team. A time out was performed. The head of bed was turned 90 degrees from anesthesia. A maxillary mouthguard was placed over the maxillary dentition. The rigid cervical esophagoscope was advanced transorally towards the hypopharynx, with the tip placed into the post-cricoid region. The scope was advanced into the cervical esophagus. There was a prominent cricopharyngeal bar due to cricopharyngeus hypertrophy. Photodocumentation was obtained with a zero-degree rigid endoscope. This was removed and the Weerda diverticuloscope was then advanced past the post-cricoid region and into the cervical esophagus. The diverticuloscope was put into suspension with a good view of the cricopharyngeal bar. A Trease injector was used to inject 1 cc of Botox (100 U/cc) into the cricopharyngeus in three locations: roughly 33 U in left, middle, and right. Starting with 46 French, Maloney dilators were then serially passed into the esophagus up to 56 French without significant difficulty. The dilators were removed and the patient was turned back over to the anesthesia team for emergence and extubation.
As per Dewan et al. (Dewan 2020) in a PubMed search for all articles about treating adult achalasia of the cricopharyngeus between 1990 to 2019 - 60 articles were selected with findings:
- Etiology
- 28% Idiopathic
- 28% Secondary to cerebrovascular accident
- 17% Due to neurologic disease
- 11% Associated with Head and Neck Irradiation
- 10% Zenker's diverticulum
- 5% Myositis
- Treatment (a portion treated with more than one approach)
- 40% Botulinum toxin injection
- 30% Endoscopic CP myotomy
- 25% Dilation with either balloon or bougie
- 15% Open CP myotomy
- Conclusions
- Complications most common in patients having Head and Neck Irradiation
- There is need for a prospective study to directly compare outcomes of treatment options
- Management of cricopharyngeal achalasia is challenging and sometimes dangerous - with risk of esophageal perforation, leak, "mediastinitis and even death"
- "To date, the literature regarding efficacy and safety of the 3 most common interventions is inconclusive"
References
Dewan K, Santa Maria C, Noel J. Cricopharyngeal Achalasia: Management and Associated Outcomes-A Scoping Review. Otolaryngol Head Neck Surg. 2020 Jun 23:194599820931470. doi: 10.1177/0194599820931470. Epub ahead of print. PMID: 32571156.
Taira K, Yamamoto T, Mori-Yoshimura M, Sajima K, Takizawa H, Shinmi J, Oya Y, Nishino I, Takahashi Y. Cricopharyngeal bar on videofluoroscopy: high specificity for inclusion body myositis. J Neurol. 2021 Mar;268(3):1016-1024. doi: 10.1007/s00415-020-10241-7. Epub 2020 Sep 26. PMID: 32980980.
Klingler MJ, Landreneau JP, Strong AT, Barajas-Gamboa JS, Tat C, Tu C, Fathalizadeh A, Kroh M, Rodriguez J, Sanaka MR, Ponsky J. Endoscopic mucosal incision and muscle interruption (MIMI) for the treatment of Zenker's diverticulum. Surg Endosc. 2021 Jul;35(7):3896-3904. doi: 10.1007/s00464-020-07861-5. Epub 2020 Aug 6. PMID: 32748264.
Hoffman MR, Kletzien H, Dailey SH, McMurray JS. Simulation of KTP Laser-Based Zenker Diverticulotomy with a Porcine Model and Laryngeal Dissection Station. OTO Open. 2017 Dec;1(4):2473974X17736288. doi: 10.1177/2473974X17736288. Epub 2017 Oct 16. PMID: 29350715; PMCID: PMC5751941.